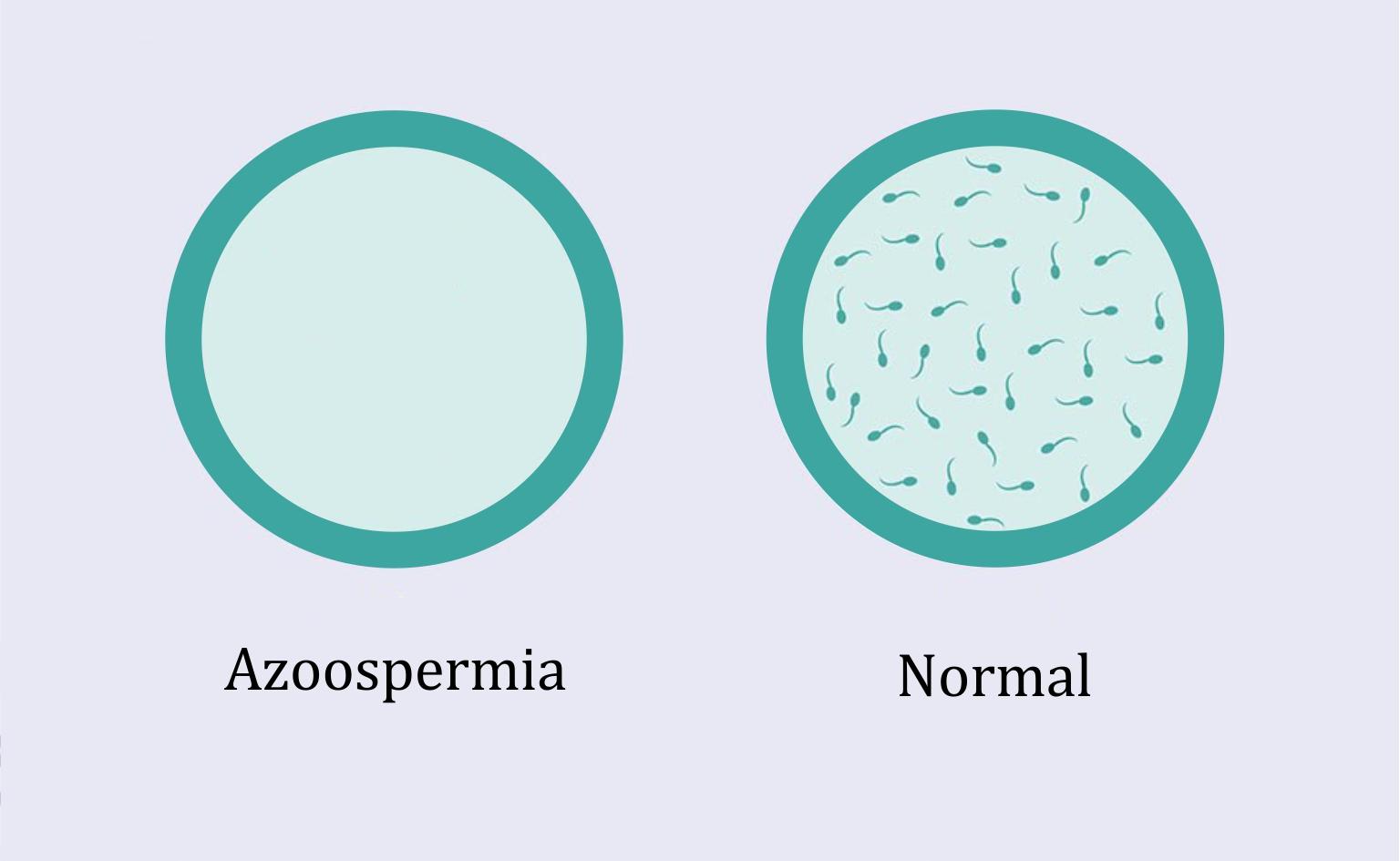
Natural pregnancy in a woman whose partner has secretory or obstructive azoospermia is not possible. However, when the treatments applied do not solve the problem, Dawasanté experts offer you a natural herbal treatment to cure your azoospermia and allow your partner to quickly get pregnant.
Click here or on the image below to discover this natural treatment .
To discover our natural solution to treat azoospermia click here!
Contact our experts, tel / WhatsApp: +22990312738
1: Aspiration of sperm
In men with obstructive azoospermia , no sperm is seen in the ejaculate, but sperm is produced in the testis.
One option is to extract the sperm directly from the testis or epididymis. In this way, it is possible to obtain sperm, but in low quantity and of poor quality in relation to mobility and morphology.
For this reason, in the event of obtaining sperm by aspiration, it will be necessary to resort to the technique of ICSI (intracytoplasmic sperm micro-injection). ICSI is the ideal in vitro fertilization technique because only one sperm is needed for each egg to be fertilized. In addition, in this process, it is the specialist himself who introduces the sperm into the egg.
There are several procedures for extracting sperm, and their names come from the acronyms in English:
1.1: MESA
Corresponds to the term: microsurgical epididymal sperm aspiration , i.e., microsurgical aspiration of epididymal sperm. It is used in patients with obstruction of the genital tract. This involves making a small incision in the epididymis and extracting the sperm from inside the epididymis.
It is a complicated operation and the costs are high. For this reason, although it allows to collect more sperm than with a PESA, it is not the most chosen technique.
1.1.1: PESA
It is the percutaneous aspiration of epididymal sperm ( percutaneous epididymal sperm aspiration ). This is a simpler and less invasive procedure than the previous one and does not require as many skills on the part of the doctor. It is performed under sedation, so that the patient does not feel any pain.
A needle is inserted through the skin of the scrotum to reach the epididymis. The downside is that the needle is inserted blind, and although this is unusual, it is possible that no sperm will be aspirated.
1.1.2: TESA
Its English name is: testicular sperm aspiration , and it is referred to as the aspiration of sperm from the testis. It is also performed percutaneously, just like PESA. The difference is that the aspiration is done from the testes and not from the epididymis.
This type of aspiration is usually performed when the other options (MESA and PESA) are not applicable due to changes such as absence or obstruction of the epididymis.
2: Testicular biopsy
Also known as TESE ( testicular sperm extraction ). It is performed under local anesthesia and consists of the following elements:
- The specialist opens the different testicular layers using a scalpel or a laser until it reaches the testicle, from which he will extract small pieces. About 2-3 cm of testicular layers are opened. They will then be closed with one or two stitches.
- After the biopsy is performed or at the same time as the biopsy, the tissues are analyzed under a microscope for sperm, which will then be used in the ICSI technique in the hope of pregnancy.
- Although it is indicated in patients with obstructive azoospermia , it is also applied in certain situations of secretory azoospermia. In many of these cases, although no sperm is produced in the testes, foci of spermatogenesis can be found, that is, if you search exhaustively, it is possible to find a sperm.
- In any case, the possibility of achieving pregnancy by applying ICSI with the few sperm found after testicular biopsy of patients with secretory azoospermia is low.
3: Sperm donation
The above procedures may be effective for obstructive azoospermia , but they are not usually applied to secretory azoospermia. In patients with this alteration, where no treatment is able to reverse spermatogenesis, it is recommended to resort to sperm donation .
This is artificial insemination or in vitro fertilization with sperm donated by a healthy young man . This donor is subjected to a series of physical and psychological examinations to verify his good state of health and to confirm the safety of the use of his sperm.
The choice of one or the other reproductive technique will depend on certain qualities of the woman such as her age, the patency of the fallopian tubes, etc.
This is an alternative with a high probability of success . However, it has a major drawback: humans give up transmitting their genetic heritage. This means that the children born will not be the biological children of their father, since they will inherit the traits of the donor who gave the sperm.
4: Your frequently asked questions
If my husband has total azoospermia, should we consider donating sperm as the only option so that I can get pregnant?
If as total azoospermia you hear irreparable secretory azoospermia, yes, sperm donation is the best option for you to achieve pregnancy.
In severe cases of secretory azoospermia, it is very difficult to obtain viable sperm with fertilizing ability, so it is necessary to resort to sperm donation.
After 11 years of vasectomy, will I be able to have children if I have a testicular biopsy?
A testicular biopsy is used to obtain sperm directly from the testis, which is the place of production. However, after so long a time of voluntary obstruction, that is, after preventing the produced sperm from coming out, it is possible that the organism itself has reduced production. However, since only one sperm per egg is needed for ICSI treatment, you may be able to achieve pregnancy in your partner from the sperm found during the biopsy.
In any case, you should be aware that it is quite possible that no viable sperm will be found after the biopsy.
Pregnancy was detected by measuring serum HCG on two independent occasions, at least 15 days after the embryo replacement. Clinical pregnancy was determined by observing a gestational sac with a fetal heartbeat on a transvaginal ultrasound at 6–7 weeks gestation. The clinical embryo implantation rate was defined as the number of gestational sacs seen during ultrasound screening at 6-7 weeks gestation divided by the number of embryos transferred.
To discover our natural solution to treat azoospermia click here!
Contact our experts, tel / WhatsApp: +22990312738