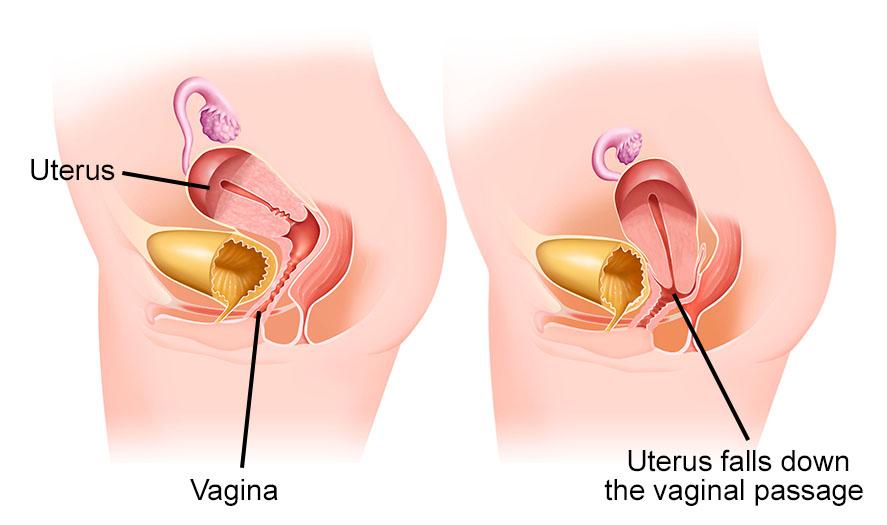
Genital prolapse is what is commonly called organ descent. The pelvic floor can be weakened by the distension of the muscles and ligaments of the perineum following childbirth, surgery, menopause. It can affect the descent of the bladder, uterus, and rectum alone or simultaneously.
To treat this disease, Dawasanté experts provide you with a natural treatment based on the best African plants. Click on the image below to discover this natural treatment
How The Prolapse Diet May Affect Your Pelvic Floor
Your diet can certainly have an impact on your prolapse.
· Diet contributes to abdominal fat - the more abdominal body fat you carry, the greater the load on your pelvic floor.
· Diet influences bowel movements - constipation and diarrhea can lead to straining and worsen prolapse problems.
· Diet can cause abdominal bloating, gas, and IBS - abdominal bloating, gas, and IBS (irritable bowel syndrome) can cause discomfort and worsen symptoms of prolapse.
1. How to lose abdominal fat for prolapse management
Your belly fat is not the fat you feel around your waist, rather it surrounds your abdominal organs and sits directly above your pelvic floor.
Abdominal fat increases the load on your pelvic floor and prolapse, which worsens your prolapse symptoms and increases your risk for the prolapse to worsen over time.
This is why it is important to avoid unnecessary weight gain or weight loss if you are overweight if you have prolapse issues and after prolapse surgery.
If you are overweight, you will be able to better manage your prolapse by losing abdominal fat.
Diet to lose abdominal fat with prolapse problems
Unfortunately, you cannot reduce abdominal fat through diet. To lose belly fat naturally requires a bodyweight reduction approach.
Here are some simple weight management tips for losing belly fat:
· Avoid diets or weight loss products in fashion (eg some diet shakes) that slow your stools and cause constipation with prolapse
· Do not skip meals - eating stimulates the stool
· Avoid artificial sweeteners that can cause gas and impact your stool.
· Drink enough water and fluids at low energy - your fluid intake affects your stool.
· Avoid snacking late at night before going to bed - your metabolism slows while you sleep
· Record what you eat and drink - you might be surprised at what you consume
· Watch your food intake accidental - it is very easy to snack when preparing food for others
· The Australian Guide to Healthy Eating provides current factual information on the types and quantity of foods to reduce the risk of diet-related problems, including obesity and high cholesterol and chronic diseases, including certain cancers, diabetes and heart disease
Abdominal and Prolapse Weight Loss Exercise
Some women are very concerned that they will not be able to exercise to manage their weight if they have a prolapse.
Fortunately, most women with prolapse issues can exercise effectively to manage their weight, avoid gaining weight or lose weight.
Studies show that women can exercise to reduce belly fat by alternating high and low-intensity exercise.
Tips for abdominal weight loss in case of prolapse:
· Keep weight management simple, ie. Weight management = energy in (food) - energy used (exercise / physical activity)
· Calculate your energy needs (food) using this simple daily energy needs calculator
· Include low-impact fitness exercises pelvic floor in your normal routine
Include weight loss exercises that prevent worsening prolapse into your regular exercise routine
· Choosing high and low-intensity alternating workouts are the best abdominal fat weight loss exercises.
2. Diet and constipation
Constipation and exertion cause and worsen prolapse problems.
If your bowel is slow, you may be familiar with the heavy feeling of prolapse and the feeling of dragging that can accompany constipation.
Women with rectocele (prolapse of the back wall of the vagina) are particularly vulnerable to constipation.
Solutions for diet and constipation with prolapse
Try to get the right stool consistency first.
Aiming for a loose, well-shaped stool is essential to help you empty your bowels without straining or making the prolapse worse.
The ideal stool consistency for bowel emptying with prolapse problems is type 3-4 on the Bristol Stool Chart
Diet and consistency of stool
Foods that soften the stool include:
· Vegetables - green beans, spinach, red pepper, garlic, green beans
· Fresh fruits with skins - stone fruits (eg apricots, peaches, plums) raisins, prunes
· Cereals rich in fiber - bran, multigrain bread, and whole grains
· Snacks - Popcorn, Chocolate
· Coffee and tea
· Spices, eg. Ex. Chili, curry
* May cause abdominal bloating
Avoid the common mistake of consuming too much fiber!
Eating too much fiber, especially insoluble fiber (eg, fruit and vegetable skins, seeds), can make constipation and bloat worse. This will often worsen the symptoms of prolapse towards the end of the day.
Dietary fiber is important for good stool consistency.
Most women should aim for 25-30 grams per day.
Consistency of fluids and stools
Some women don't drink enough fluids to help them manage the consistency of their stools, especially when increasing their fiber intake or taking fiber supplements.
Most women should aim for around 2 liters (67 oz) of water on average, but it can vary.
Some women with certain medical conditions need to limit their fluid intake and these women need to be careful to prevent too much fiber from causing a slow bowel.
Fluids that promote bowel movements include:
Water
Certain fruit juices: pear, prune, or grape
· Coffee and tea
· Alcohol
Eat breakfast to stimulate your gut. Sometimes a hot drink in the morning and getting moving can help promote bowel movements.
3. Diet and chronic diarrhea
Women with frequent bowel movements are also at risk for pelvic floor fatigue and worsening prolapse problems.
If you suffer from chronic diarrhea or loose stools, it may be beneficial to avoid or limit some of the foods and drinks mentioned above that soften the stool.
Foods that firm up stool include:
White cereals - white rice, white pasta, white bread
Cheese
Bananas
Tapioca
White marshmallows
· Pretzels
4. Diet and abdominal bloating or gas with prolapse
Abdominal bloating and / or gas can be a huge problem for women with prolapse issues.
Some women find that at the end of the day their abdomen is so swollen that their stomachs are strained and their prolapse causes abdominal pain and pelvic floor drag and bulge.
Pushing down and forcing the gas through with prolapse can make prolapse problems worse.
Bloating can be caused by my many dietary factors; some foods are not absorbed well in the gut, so they ferment to produce more gas than others, causing abdominal bloating.
Diet solutions for bloating and prolapse
Some women have IBS issues which cause poor intestinal digestion of certain foods causing bloating, excessive gas or wind, abdominal pain as well as constipation, and / or diarrhea.
When combined with prolapse, IBS can make the management of the prolapse and the discomfort very difficult.
Scientific studies have shown that symptoms of IBS can be managed by reducing FODMAPS in the diet.
FODMAPS is an acronym for some of the sugars that are not well absorbed in the gut. These sugars produce gas and carry water into the intestine.
The low FODMAP diet can provide significant relief for women with IBS and prolapse.
Foods HIGH in FODMAPS
Here are some examples of foods that can cause bloating, gas, and discomfort:
· High Fructose - honey, apples, figs, dried fruit, syrup high fructose corn
· Oligosaccharides - legumes (such as chickpeas, lentils, beans), wheat, rye, barley, garlic, onion, leek
· Disaccharides (lactose) - milk, immature cheese (eg cottage, ricotta), yogurt
· Polylols - sweeteners containing xylitol, mannitol, sorbitol, pears, stone fruits such as avocado, plums, nectarines, cherries, prunes
Fibers, still and always fibers
In the form of fresh fruits (melon, watermelon, plum, pear, apple, fig, red fruits…), and of course market vegetables (leeks, spinach, celery, fennel, cooked artichoke, zucchini, green salad, green beans…) ). Small memo for those who do not have the "dried vegetable" or "algae" reflex: lentils, peas, broad beans, and beans of all kinds - if they are well cooked - also guarantee a considerable fiber intake, as well as unrefined starches (wheat, rice and wholemeal bread).
Cereals
Like nothing else, do not hesitate to mix a few sesame, flax or squash seeds in your soups and salads. Cooked, then served hot or cold, quinoa is also one of the transit's most loyal friends.
Iron for hardened steel perineum!
This trace element helps to store oxygen in the muscles… and therefore in the perineum. We, therefore, boost "Mister P" with large reinforcements of red meat or black pudding, shellfish and crustaceans. Memo bis for those who are vegan or allergic to organ meats: as good self-respecting algae, spirulina can serve as a joker. Without forgetting the kiwi!
Some water
You know the song: at least 1.5 liters a day. Staying hydrated is the basis to avoid having to "push" too much