PROSTATE CANCER AND RADIOTHERAPY
General
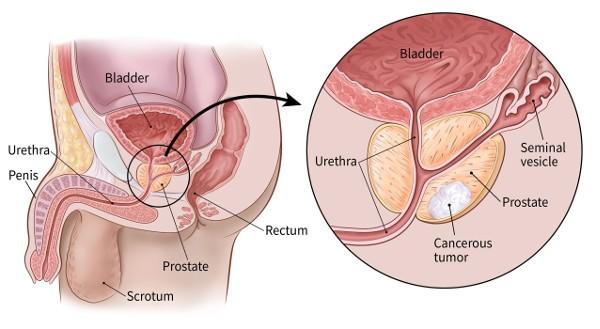
The prostate cancer is cancer frequently touching the prostate, a gland of the reproductive system of man. Cancer develops from the tissues of the prostate when cells there mutate and multiply out of control. These can then spread ( metastasize ) by migrating from the prostate to other parts of the body, especially the bones and lymph nodes in the pelvis.
Malignant prostate cancer occurs independently of benign prostatic hyperplasia (BPH), or prostatic adenoma. In the vast majority of cases, it is an adenocarcinoma, especially of the acinar type. However, Dawasanté experts have a natural African plant-based treatment to permanently cure prostate cancer and the effects of radiotherapy. Click on the image below to discover this natural treatment.
We deliver all over the world.
For more information, you can contact our experts on +229 51374202 direct line or by WhatsApp at the same number.
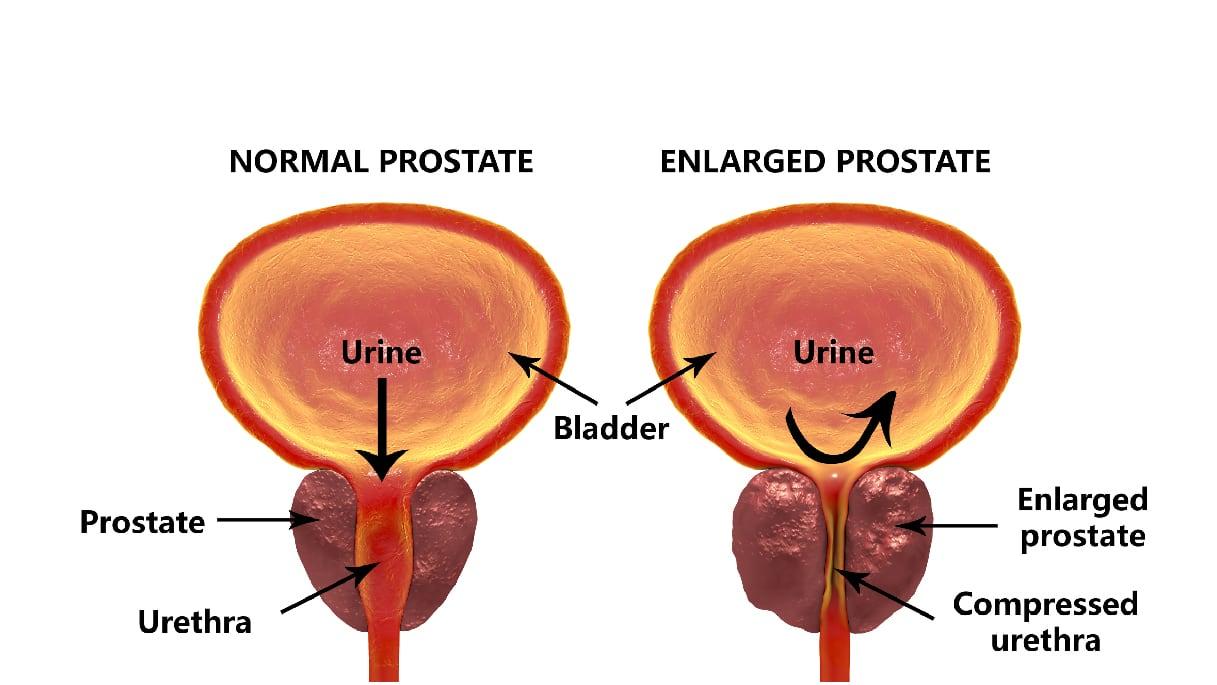
Malignant prostate cancer can cause pain, difficulty urinating, and erectile dysfunction, among other things. Symptoms originating from an adenocarcinoma of the prostate often signal an advanced stage of the disease. Other prostate diseases cause the same symptoms: pelvic pain in prostatitis and difficulty urinating in BPH.
The most common treatments are surgery (radical prostatectomy), radiotherapy ( external radiotherapy and brachytherapy, in particular) and hormone therapy. The chemotherapy is used only in advanced forms. Here we will talk about radiotherapy. However, if you feel the need to be analyzed and treated, the Dawabio center is at your disposal to provide you with a treatment worthy of the name, natural of course.
Causes, risk factors
Its causes are still poorly understood, and could often be multiple:
- a genetic predisposition and the responsibility of certain genes seem possible but weakly correlated with the onset of the disease.
In particular, a mutation on chromosome 8 could explain the greater frequency of this cancer in black Americans; - A link with bioavailable testosterone seems frequent. Charles Brenton Huggins (inventor of hormone therapy for cancer) first (from the 1940s and based on studies of metastatic prostate cancer) concluded that this cancer was induced by excess testosterone (or facilitated by this hormone). But more recently (the 2010s) the available data suggests that a more common cause is testosterone deficiency. Low testosterone before surgery for this cancer was linked in 2010 to an increased risk of tumor aggressiveness
- higher adult height correlates with a higher risk of prostate cancer;
- Nutritional factors have been mentioned. Certain foods seem to increase the risk of prostate cancer;
According to several studies, the consumption of cow's milk increases this risk after 50 years, but other studies consider that this link is not significant or would be weak. The increased risk appears to be related to the increased level of IGF-1 in the blood, which itself correlates with milk consumption. Some studies suggest that casein may also have an effect on prostate cancer. Excessive dietary intake of phytanic acid from dairy products, especially butter has also been linked (2012) to a high risk of prostate cancer; for these reasons, in the name of the precautionary principle, the consumption of dairy products is no longer recommended for men. Overconsumption of calcium appears to be an established risk factor. Several scientific studies retain milk as a risk factor for hormone-dependent cancers such as those of the prostate, ovaries and breast.
Other foods seem to play a protective role; the lycopene for example, dried fruits, legumes ;
- similarly, physical exercise may have a slightly protective effect;
- an endocrine disrupting effect of certain products ( pesticides in particular) could be involved;
- exposure to pesticides is a possible factor because agricultural populations are over-represented for this cancer, which remains etiologically poorly understood, and which therefore still requires research, in particular on gene-environment relationships and interactions . The cadmium very present in phosphate fertilizers could also be involved;
- The smoking ;
- a viral infection could sometimes be involved (unless it is favored by the process of cancerization or a decrease in immunity which also favored cancer);
the XMRV retrovirus ( Xenotropic MLV - Related Virus, variant of MLV ( murine leukemia virus responsible for leukemia in mice) and capable of infecting humans, was detected in 2006 in certain tumors of the prostate. It belongs to the gammaretrovirus genus already associated with leukemia and certain cancers in rodents, felines, and primates.
According to a US study published in 2010 and involving 334 human prostate tissue samples, proteins appearing to come from this virus were found in 23% of cancerous tissue (against 4% of "healthy" samples). And they were more present in the more aggressive tumors. It remains to be identified whether the virus is the cause or one of the causes of these cancers or if it infects the prostate of patients because they have previously weakened immunity. If it is involved, we may have additional biomarkers for this cancer or even new avenues of prevention; - The night work is also mentioned (as for other cancers called "hormone").
- according to a study published in 2004, more frequent ejaculations are associated with a reduced risk of prostate cancer.
What are its symptoms and how is it detected?
This cancer is most often asymptomatic, that is to say, it is discovered when it does not cause any manifestation of its own. It is most often found:
- during blood tests including the study of PSA (specific antigen of the prostate, whose predictive value and use, without proven benefit in terms of public health , have recently been called into question). PSA is a protein normally secreted by prostate cells, but a cancer cell secretes 10 times more than a normal cell. This property has raised many hopes in terms of screening. The blood level of PSA can however be increased by many other factors (prostate volume, infections and / or inflammations, mechanical constraints (rectal examination, other) ...) or decreased by certain treatments for benign hypertrophy ( finasteride). The significance thresholds are therefore difficult to establish. It is accepted, however, that a PSA level of between 4 and 10 ng/ml is doubtful, but that it is clearly significant beyond. Some authors have proposed to relate the rate to the effective weight of the prostate or to assess the free PSA / total PSA ratio, or even the growth kinetics of the rate over 2 years.
A still uncertain marker for screening, the PSA level is, on the other hand, an essential indicator for the monitoring and treatment of declared cancers; - during a digital rectal examination; performed routinely, or due to symptoms related to another disease (in particular benign prostatic hypertrophy);
- fortuitously, on parts of prostatic resection during the surgical treatment of prostatic adenoma.
When symptomatic, prostate cancer is most often at an advanced stage. It can lead to:
- acute urinary retention ;
- hematuria ;
- sexual impotence (erectile dysfunction);
- a deterioration of the general condition ;
- of pain and/or the malfunction or failure of other organs related to the presence of metastases .
Radiotherapy is one of the treatments conventionally offered in prostate cancer
External or internal radiotherapy?
A second option in the treatment of localized prostate cancer is radiation therapy.
Two types of radiotherapy are used to treat this pathology, external radiotherapy and internal radiotherapy also called brachytherapy or brachytherapy.
The external radiation corresponds to conventional radiation: radiation from an external source are directed so focused on the patient's tumor. The dose of radiation needed to destroy the tumor is delivered over several sessions, often five per week for one to two months.
Internal radiation therapy is based on the implantation of radioactive needles into the prostate. The needles are put in place during surgery, under general anesthesia. This method has the advantage of sparing the organs neighboring the prostate since the radioactive radiation is delivered directly into the prostate gland.
The various complications of radiotherapy are described in the chapter devoted to radiotherapy and accessible in the treatment section itself in the health section of the site.
External radiotherapy and brachytherapy are among the potentially curative therapeutic modalities offered in the treatment of non-metastatic prostate cancer. Few data have been published on their management and their prevention is essential. An assessment as precise as possible of the risk / benefit ratio is necessary before any treatment decision and clear and objective information for the patient must be made, including the risk of late morbidity and the possible impact of late side effects on quality of life.
The immediate digestive side effects during irradiation are very frequent and almost constant even if they are mostly very moderate and with limited impact. They consist of transit disorders sometimes linked to enterocolitis and accompanied by abdominal pain and above all by a rectal syndrome with a fractionation of the stools which become mucus and some false needs. Patients with hemorrhoids develop anal discomfort earlier and more readily, sometimes with bleeding and should be treated early.
Most of these side effects disappear a few weeks after the end of the irradiation.
Late complications are much rarer, around 7 to 10% for grade 1-2 complications and have become exceptional for serious complications (3.5% grade 3 and 0.5% grade 4). These late complications, when they occur, are essentially anorectal, with the risk of enteritis only occurring when large volumes of hail have been included in a large volume of pelvic irradiation. The evaluation of these complications is done according to the score, LENT SOMA (Late Effects on Normal Tissue Scale) of the RTOG-EORTC:
Grade 1: no change.
Grade 2: mild diarrhea; some colic pain; less than 5 bowel movements per day; mucus stool.
Grade 3: moderate diarrhea; more than 5 bowel movements per day; mucous or haemorrhagic proctitis.
Grade 4: obstruction or rectal bleeding requiring surgery.
Grade 5: necrosis, perforation, fistula.
Urinary complications from radiotherapy are rare even if during irradiation, irritative phenomena are very frequent. However, it is the rule not to irradiate a very large adenomatous prostate in patients with high IPSS, otherwise, a retention syndrome may occur during treatment. The removal of the previous obstacle will call for the usual medical or surgical treatments. The start of irradiation should be postponed after a transurethral resection to avoid increasing the risk of urinary incontinence or subsequent stenosis and will not begin until after complete healing of the resection pocket, generally in the third month.
We deliver all over the world.
For more information, you can contact our experts on +229 51374202 direct line or by WhatsApp at the same number.