blocked tubes solution
PREGNANCY WITH A SINGLE FALLOPIAN TUBE: natural treatment
Pregnancy is the condition of a pregnant woman. The question is whether a woman can get pregnant with just one fallopian tube. Obviously YES. Dawasanté experts offer you a natural treatment to unblock your tubes and allow you to quickly get pregnant. Click on the image below to discover this natural treatment
PREGNANCY WITH A SINGLE BLOCKED FALLOPIAN TUBE
Is it possible for me to get pregnant if I only have one fallopian tube?
Uterine tubes (or fallopian tubes) are muscle tubes leading from the ovaries to the uterus. The uterine tubes are responsible for collecting the egg each month. The fusion between the egg and the sperm (fertilization) also takes place inside the egg. The resulting embryo is taken to the uterus where the pregnancy will progress. Obviously, the fallopian tubes play an essential role in natural reproduction linked to ovulation, fertilization and pregnancy. Diseases or abnormalities of the uterine tubes are responsible for up to 30% of infertility cases.
What if I have blocked tubes and want to get pregnant?
Here is the best African herbal remedy to unblock the tubes and get pregnant quickly. These herbs are very effective in unblocking the fallopian tubes. They have already enabled many women around the world who had blocked tubes to regain their fertility without operations. If you have blocked tubes, here are the medicinal plants that will allow you to experience the joy of being a mother.
To discover our natural remedy to unblock the tubes and get pregnant quickly, Click on the image
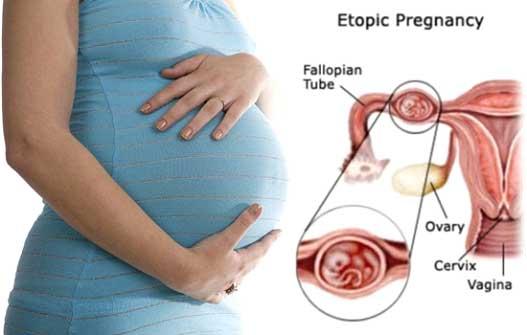
The anatomical integrity of the fallopian tubes is essential for natural fertility. Many health conditions can affect the fallopian tubes. For example, an ectopic pregnancy (pregnancy outside the womb in one of the fallopian tubes). Surgery and removal of the affected tube are often necessary for such conditions for these to be properly thinned. Questions arise after surgery: Will I be able to get pregnant naturally if I only have one fallopian tube? The answer is yes, although the chances of conceiving naturally decrease slightly. Some research estimates this decrease between 15 and 45%.
There are other diseases, as well as ectopic pregnancies, which can damage one or both fallopian tubes. For example, endometriosis, sexually transmitted diseases and abdominal surgery (appendicitis and peritonitis, among others). If both tubes are affected (or if they have been removed), natural conception is highly unlikely and appropriate treatment will include assisted reproduction therapy through in vitro fertilization in order to achieve pregnancy.
Have only one fallopian tube. Is it possible for me to get pregnant?
Yes. The fallopian tubes are a pair of tubes through which eggs pass from the ovaries to the uterus. Each month, in a process called ovulation, one of the ovaries releases an egg that travels to one of the fallopian tubes, where it may or may not be fertilized by a sperm.
You may only have one fallopian tube if you've had pelvic surgery for an infection, tumor, or ectopic pregnancy. Sometimes some women are born with just one tube. However, you can still be pregnant with just one tube if:
You have at least one working ovary
You have monthly menstrual cycles (ovulation)
Your remaining fallopian tube is healthy
If you are unable to get pregnant after trying to conceive or have a known history of fallopian tube problems, see your gynecologist or reproductive endocrinologist for evaluation.
HERE ARE SOME TIPS TO FIGHT AGAINST CLOUDY TRUMPS
1-Turmeric
Turmeric is a natural anti-inflammatory. It can be very effective in unblocking the fallopian tubes. Curcumin, the active ingredient in turmeric, is very effective in reducing inflammation. You can consume curcumin in supplement form, add turmeric to your food, or drink a glass of turmeric.
Turmeric has no known side effects when taken in small doses. However, at doses of more than 8 grams per day, it can have unwanted effects. Make sure you take the correct dosage of turmeric or, better yet, add the spice to your cooking.
2-Garlic
Garlic is a great way to improve fertility and unclog fallopian tubes. Garlic has always been consumed for its many health benefits as the aphrodisiac properties present in garlic help in improving blood circulation in the body. Eating raw garlic every day on an empty stomach helps fight infertility in women, lowers blood pressure and cholesterol.
3-Vitamin C
Vitamin C is an antioxidant that can reduce inflammation by helping your immune system to function better. For this reason, it is ideal for healing scars and may have a positive effect on the fallopian tubes.
If you suspect that the cause of the blocked fallopian tubes is an infection, vitamin C can help you overcome it. To unclog your tubes, we recommend that you use natural vitamin C. It's easy to get vitamin C from food sources, especially when you like citrus fruits. Eat as many oranges, lemons, and grapefruit as possible. Aside from, you can try strawberries, broccoli, and green peppers to cure yourself with good vitamin C.
4- Castor oil
Castor oil has been used for centuries to improve fertility in women, and more specifically to unblock the fallopian tubes. How is it used?
- dipped a rag in castor oil
-Place this cloth on the skin on the lower abdomen. This will improve circulation and promote healing of the tissues and organs under the skin. Castor oil therapy helps the fallopian tubes by softening tissue and improving circulation in the pelvic area.
5- Apple cider vinegar
Apple cider vinegar is a fermentation product that produces yeasts and bacteria that are beneficial for unblocking the tubes. This is because vinegar contains a number of vitamins and minerals, including magnesium, potassium, copper, group B vitamins and vitamin C. Taken daily, it can help unblock the fallopian tubes by balancing hormones and shrinking fibroids.
Manual:
-Mix 2 tablespoons of apple cider vinegar in 1 glass of water
-You can add a touch of honey or molasses to sweeten the mixture.
-You can drink the mixture right away or sip it for 30 minutes.
6-Meditation
Meditating daily will help lower stress levels and promote general healing. However, reducing stress reduces deterioration and inflammation of the fallopian tubes.
As an additional tip, don't forget to start meditating with a short session consisting of breathing exercises and relaxation techniques. Even if you only do it for a few minutes, meditation will provide you with positive energy to start your day and reduce your stress.
Because of the high number of eggs that just one of your ovaries can make, your chances of getting pregnant again are almost as great as before this procedure. The only problem is that there may be a small anomaly in the second proboscis. It may therefore be necessary to do some examinations to check that it is perfectly permeable. Your gynecologist will tell you if he deems these exams necessary. But whatever your situation, technical advancements in this area suggest that your chances of becoming a mother in the future remain intact.
PELVIC INFLAMMATORY DISEASE
The pelvic inflammatory disease , or PID, is the term used for generalized inside infection of the uterus, fallopian tubes and ovaries. Symptoms of PID can include vaginal discharge, chronic pelvic pain, and fever. However, Dawasanté experts have available a treatment to remedy this disease. Click on the image below to discover this natural treatment
PELVIC INFLAMMATORY DISEASE
GENERALITY
Inflamed pelvic inflammatory disease fallopian tubes
Pelvic inflammatory disease (PID) is an infection of the reproductive organs of women. This usually happens when sexually transmitted bacteria spread from the vagina to the uterus, fallopian tubes, or ovaries.
If you suffer from pelvic inflammatory disease click here
Pelvic inflammatory disease often does not cause any signs or symptoms. As a result, you may not realize that you have the disease and get the treatment you need. The condition can be detected later if you are having trouble getting pregnant or if you develop chronic pelvic pain.
What if I have blocked tubes or PID and want to get pregnant?
Symptoms
The signs and symptoms of pelvic inflammatory disease can include:
Pain in the lower abdomen and pelvis
Heavy vaginal discharge with an unpleasant odor
Abnormal uterine bleeding, especially during or after sex, or between menstrual cycles
Pain or bleeding during sex
Fever, sometimes with chills
Painful or difficult urination
The MIP can cause only mild signs and symptoms, if any. When severe, PID can cause fever, chills, severe abdominal or pelvic pain - especially during a pelvic exam - and bowel discomfort.
When to see a doctor
See your doctor or seek urgent medical attention if you have:
Severe pain in the abdomen
Nausea and vomiting, with an inability to keep anything
Fever, with a temperature over 101 F (38.3 C)
Vaginal discharge
If your signs and symptoms persist but are not serious, see your doctor as soon as possible. A discharge from the vagina with an odor, painful urination, or bleeding between menstrual cycles may be associated with a sexually transmitted infection (STI). If these signs and symptoms appear, stop having sex and see your doctor soon. Prompt treatment of an STI can help prevent PIDs.
The causes
Many types of bacteria can cause PIDs , but gonorrhea or chlamydia infections are the most common. These bacteria are usually acquired through unprotected sex. Less commonly, bacteria can enter your reproductive tract whenever the normal barrier created by the cervix is disrupted. This can happen after childbirth, miscarriage, or abortion.
Risk factors
A number of factors can increase your risk for pelvic inflammatory disease, including:
Be a sexually active woman under 25
Having multiple sexual partners
Being in a sexual relationship with someone who has more than one sexual partner
Having sex without a condom
Showering regularly, which upsets the balance of beneficial and harmful bacteria in the vagina and may mask symptoms
Having a history of pelvic inflammatory disease or sexually transmitted infection
Most experts now agree that an inserted intrauterine device (IUD) does not increase the risk of pelvic inflammatory disease. Any potential risk is usually within the first three weeks after insertion.
Complications
Untreated pelvic inflammatory disease can cause scar tissue. You could also develop collections of infected fluid (abscess) in the fallopian tubes, which could damage your reproductive organs.
Other complications can include:
Ectopic pregnancy. The PID is a major cause of tubal pregnancy (ectopic). In an ectopic pregnancy, the scar tissue from the PID prevents the fertilized egg from making its way through the fallopian tube to implant in the uterus. Ectopic pregnancies can cause massive, life-threatening bleeding, and require urgent medical attention.
Infertility. PID can damage your reproductive organs and cause infertility - the inability to get pregnant. The more PID you have had, the greater your risk of infertility. Delaying treatment for PIDs also greatly increases your risk of infertility.
Chronic pelvic pain. Pelvic inflammatory disease can cause pelvic pain that can last for months or even years. The scarring in the fallopian tubes and other pelvic organs can cause pain during intercourse and ovulation.
Tubo-ovarian abscess. The MIP can cause the formation of an abscess - a collection of pus - in the fallopian tube and ovaries. If left untreated, you could develop a life-threatening infection.
Prevention
To reduce your risk of pelvic inflammatory disease:
Practice safe sex. Use condoms every time you have sex, limit the number of partners, and ask about a potential partner's sexual history.
Talk to your doctor about contraception. Many forms of contraception do not protect against the development of PID . Using barrier methods, such as a condom, can help reduce your risk. Even if you are taking birth control pills, it is still important to use a condom every time you have sex to protect yourself from STIs.
Have it tested. If you're at risk of getting an STI, such as chlamydia, make an appointment with your doctor for a screening test. Establish a regular screening schedule with your doctor if necessary. Treating an STI early gives you the best chance of avoiding PID.
Request that your partner be tested. If you have pelvic inflammatory disease or an STI, ask your partner for a screening test and, if necessary, treatment. This can prevent the spread of STIs and the possible recurrence of PIDs .
Pelvic inflammatory disease is a polymicrobial infection of the female genital tract: cervix, uterus, fallopian tubes, and ovaries; an abscess can form. Pelvic inflammatory disease can be sexually transmitted. Symptoms usually include abdominopelvic pain, cervical discharge, and irregular bleeding. Long-term complications include infertility, chronic pelvic pain, and ectopic pregnancy. Diagnosis is made by PCR of cervical swabs for Neisseria gonorrhoeae and Chlamydia, microscopic examination of cervical discharge (usually), and ultrasound or laparoscopy (sometimes). Treatment is based on antibiotics.
Pelvic inflammatory disease can affect the cervix, uterus, fallopian tubes, and / or ovaries. Infection of the cervix ( cervicitis ) causes mucopurulent discharge. Infections of the fallopian tubes (salpingitis), uterus (endometritis), and ovaries (oophoritis) tend to occur at the same time. If severe, the infection can spread to the ovaries (oophoritis) and then to the peritoneum (peritonitis). Salpingitis with endometritis and oophoritis, with or without peritonitis, is often called salpingitis, although other structures are involved. Pus may collect in the tubes (pyosalpinx) and an abscess may form (tubo-ovarian abscess).
Etiology
Pelvic inflammatory disease is caused by an overgrowth of organisms that originate from the vagina and cervix and travel up into the uterus and fallopian tubes. Neisseria gonorrhoeae and Chlamydia trachomatis are common causes of pelvic inflammatory disease; they are sexually transmitted. Mycoplasma genitalium , which is also transmitted sexually, can also cause or contribute to pelvic inflammatory disease. The incidence of sexually transmitted inflammatory pelvic disease is decreasing; to <50% of patients who have a positive acute pelvic inflammatory disease test for gonorrhea or chlamydia infection.
Pelvic inflammatory disease usually also involves other aerobic and anaerobic bacteria, including bacterial vaginitis pathogens . Vaginal organisms such as Haemophilus influenzae , Streptococcus agalactiae , enteric gram-negative bacilli may be involved in pelvic inflammatory disease, as well as Ureaplasma sp. Vaginal inflammation and bacterial vaginosis contribute to the upward spread of vaginal organisms.
Risk factors
Pelvic inflammatory disease is seen in women <35 years old. It is rare before the first period, after menopause and during pregnancy.
Risk factors include
-
History of pelvic inflammatory disease
-
Presence of bacterial vaginitis or any sexually transmitted infection
Other risk factors, especially for pelvic inflammatory gonococcal disease or Chlamydia, include
-
Young age
-
Non-white race
-
Low socioeconomic status
-
Multiple or new sex partners
-
Vaginal irrigations
Symptomatology
Abdomino-pelvic pain, fever, leucorrhoea and functional menometrorrhagia are common, especially during or after menstruation.
Cervicitis
In cervicitis, the cervix is red and bleeds easily. Mucopurulent leucorrhoea are frequent; usually they are yellow-green and can be seen draining from the endocervical canal.
Acute salpingitis
Abdomino-pelvic pain is usually present and bilateral but can be unilateral, even if both tubes are affected. Pain can also be felt in the upper abdomen. Nausea and vomiting are common when the pain is severe. Metrorrhagia (caused by endometritis) and fever appear in up to 1/3 of patients.
In the early stages, symptoms may be mild or absent. Later, sensitivity to cervical mobilization, muscle defense and increased decompression pain are common.
Sometimes dyspareunia or dysuria are observed.
Many women with inflammation severe enough to cause scarring have little or no symptoms.
Pelvic inflammatory disease caused by N. gonorrhoeae is usually more acute and causes more severe symptoms than that caused by C. trachomatis , which can be indolent. Pelvic inflammatory disease caused by M. genitalium , like that caused by C. trachomatis , is also mild and should be considered in women who do not respond to first-line therapy for pelvic inflammatory disease.
Complications
The Fitz-Hugh-Curtis syndrome (périhépatite causing pain right upper quadrant) can result from pelvic inflammatory disease gonorrhea or chlamydia. The infection can become chronic, with exacerbations and intermittent remissions.
A tubo-ovarian abscess (collection of pus in the appendages) develops in about 15% of women who have salpingitis. It can accompany an acute or chronic infection and is more likely in the event of treatment delay or incomplete treatment. Pain, fever, and peritoneal symptoms are usually present and can be severe. An adnexal mass may be palpable, although extreme pain may limit the possibilities for examination. The abscess can rupture, causing progressively severe symptoms and sometimes septic shock.
The hydrosalpinges (distension fluid by tubal obstruction flag of tubes) is usually asymptomatic, but may be responsible for pelvic gravity, chronic pelvic pain or dyspareunia and / or infertility.
Salpingitis can lead to scarring and adhesion of the tubes, which often results in chronic pelvic pain, infertility, and an increased risk of ectopic pregnancy.
Diagnostic
-
Strong suspicion
-
PCB
-
Pregnancy test
Pelvic inflammatory disease is suspected when women of childbearing age, especially those with risk factors, have lower abdominal pain or unexplained cervical or vaginal discharge. Pelvic inflammatory disease is suggested when irregular bleeding, dyspareunia, or dysuria remains unexplained. Pelvic inflammatory disease is more likely in cases of abdomino-pelvic pain, unilateral or bilateral adnexal pain, and pain when the cervix is mobilized. A palpable adnexal mass suggests a tubo-ovarian abscess. A pauci-symptomatic infection can leave serious consequences, caution must be exercised.
If pelvic inflammatory disease is suspected, cervical swabs analyzed by PCR for N. gonorrhoeae and C. trachomatis (with sensitivity and specificity of approximately 99%) and a pregnancy test is performed. If PCR is not available, cultures are performed. However, infection of the upper tract is possible even with negative cervical swabs. At this time, the cervical discharge is usually examined to confirm the presence of pus; a Gram stain or an examination on a wet mount under physiological serum is carried out but these examinations are neither sensitive nor specific.
If a patient cannot be seen because of pain, an ultrasound is done as soon as possible.
The white blood cell count may be high but is not helpful for diagnosis.
If the pregnancy test is positive, an ectopic pregnancy, which may cause similar symptoms, should be considered.
Other common causes of pelvic pain include endometriosis, adnexal torsion, ruptured ovarian cyst, and appendicitis. The signs that differentiate these disorders are discussed elsewhere ( Pelvic pain ).
Fitz-Hugh-Curtis syndrome can resemble acute cholecystitis but can usually be differentiated by finding salpingitis during pelvic examination and, if necessary, on ultrasound.
If an adnexal or pelvic mass is suspected clinically or if a patient does not respond to antibiotics within 48 to 72 h, ultrasound is done as soon as possible to rule out tubo-ovarian abscess, pyosalpinx and unrelated disorders. pelvic inflammatory disease (eg, ectopic pregnancy , adnexal torsion ).
If the diagnosis is uncertain after ultrasound, a laparoscopy should be performed; purulent peritoneal fluid observed laparoscopically is the gold standard for diagnosis.
Treatment
-
Antibiotics to cover N. gonorrhoeae , C. trachomatis , and sometimes other organisms
Antibiotics are administered empirically to cover N. gonorrhoeae and C. trachomatis and are secondarily adjusted to the results of the antibiogram. Empiric treatment is necessary whenever the diagnosis is in question for several reasons:
-
Tests (especially bedside tests) are inconclusive.
-
Diagnosis based on clinical criteria may be imprecise.
-
Failure to treat mildly symptomatic pelvic inflammatory disease can lead to serious complications.
Hospitalization of the patient with cervicitis or clinically mild to moderate pelvic inflammatory disease is not necessary. The outpatient treatment protocol aims ( Protocols for the treatment of pelvic inflammatory diseases * ) usually also to eradicate bacterial vaginitis , which often coexists.
Sexual partners of patients infected with N. gonorrhoeae or C. trachomatis should be treated.
If patients do not improve after treatment that covers the usual pathogens, pelvic inflammatory disease due to M. genitalium should be considered. Patients can be treated empirically with moxifloxacin 400 mg po once / day for 7 to 14 days (eg, for 10 days).
Women with pelvic inflammatory disease are usually hospitalized if any of the following signs are present:
-
Uncertain diagnosis, with inability to rule out a disorder requiring surgical treatment (eg, appendicitis)
-
Pregnancy
-
Severe symptoms or a high fever
-
Tubo-ovarian abscess
-
Inability to tolerate or follow outpatient treatment (eg, due to vomiting)
-
Lack of response to outpatient (oral) treatment
In these cases, IV antibiotics ( Treatment protocols for pelvic inflammatory diseases * ) are started as soon as the bacteriological samples are taken and are continued until the patient is afebrile for 24 h.
The tubo-ovarian abscess may require a more prolonged IV antibiotic therapy. Treatment with transvaginal or percutaneous drainage guided by ultrasound ultrasound or CT may be considered if the response to antibiotics alone is incomplete. Sometimes a laparoscopy or a laparotomy is necessary for drainage. If a ruptured tubo-ovarian abscess is suspected, immediate laparotomy is necessary. In women of childbearing age, surgery should be aimed at preserving the pelvic organs (in the hope of preserving fertility).