hyperplastic polyp
UTERINE POLYPS AND CANCER: Natural treatment
UTERINE POLYPS AND CANCER
A polyp can sometimes seem like a fibroid uterus ( polyp fibrous) or cancer endometrial ( polyp atypical, irregular). Conversely, cancer endometrial can sometimes look like a polyp. The combination of a polyp to cancer endometrial is more common after menopause. However, Dawasanté experts provide you with a natural treatment to cure uterine polyp cancer. Click on the image below to discover this natural treatment.
To contact our experts please call or write to us on the following number, tel / WhatsApp: https://wa.me/22996374527
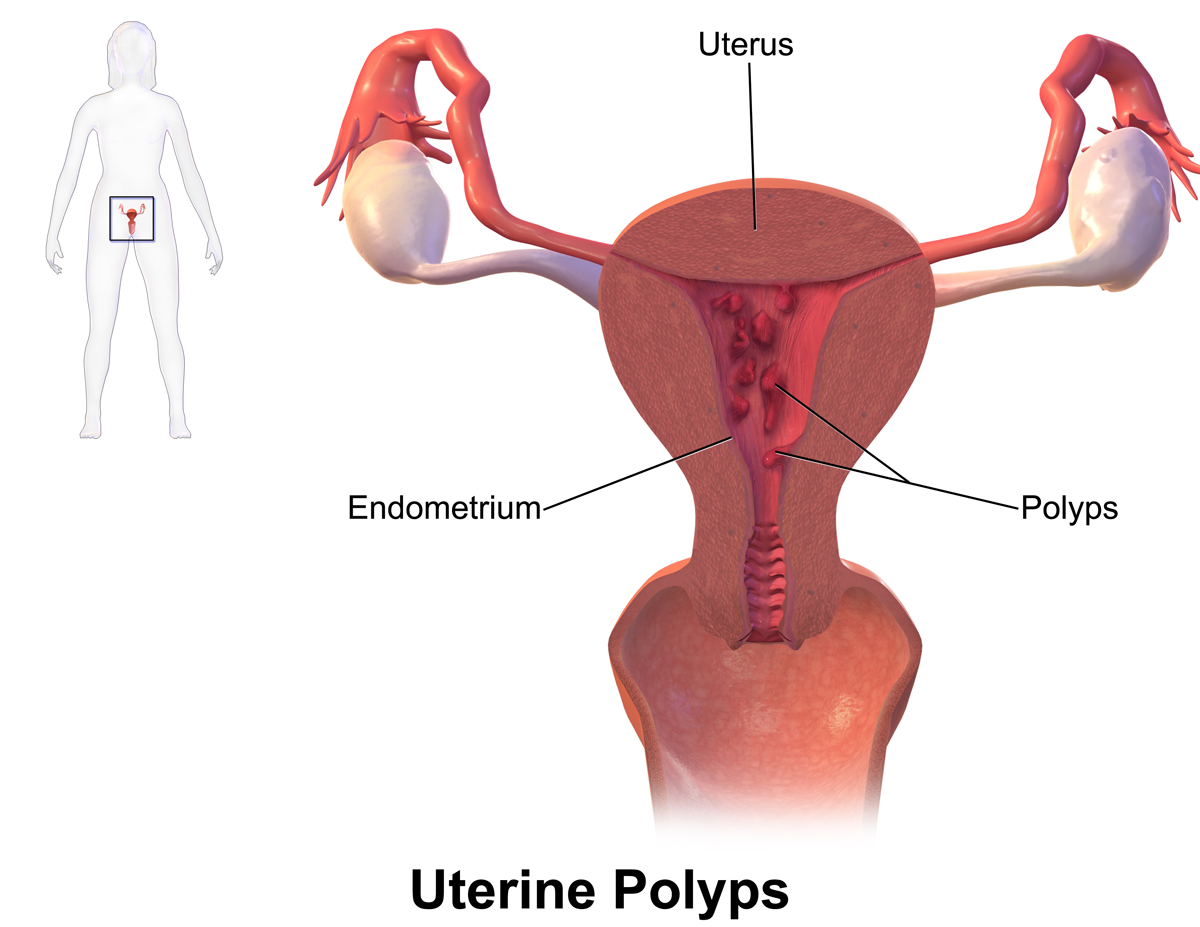
The uterine polyps are growths that develop at the expense of the lining of the uterus (endometrium), or at the expense of the lining of the cervix (endocervical).
These growths are benign tumors. They can be single or multiple. A polyp can be "pedicle" (comprising an insertion foot) or sessile (broad implantation base). It can be "fibrous" or "mucous". By definition, the development of a polyp occurs at the expense of a mucous membrane. This is why, in addition to the uterus, certain organs or areas of the human body can be invaded by this type of tumor such as the bladder, colon, stomach, vagina, etc.
The uterine polyps are outgrowths attached to the inner wall of the uterus which extends into the uterine cavity. Cellular proliferation in the lining of the womb (endometrium) results in the formation of uterine polyps, also called endometrial polyps. These polyps are usually non-cancerous (benign), although some can be cancerous or turn into cancer (precancerous polyps).
A uterine polyp can look like a fibroid or a cancerous tumor, so be careful not to get the wrong diagnosis. Cancerization of the polyp is possible.
All examinations performed should show whether the uterine polyps are benign or not. Thus, after removing these growths, a complete analysis of them is required. Postmenopausal women are prone to endometrial cancer combined with uterine polyps.
Two forms of treatment are possible to treat polyps, the choice is based on their benignity, size, appearance, etc. Those that are small and less worrying may go away as a result of hormonal drug therapy. With this treatment, the patient takes progestins. In most cases, operative hysteroscopy is necessary, it consists of the removal of the polyps. This form of treatment should be carried out with great care, especially in women who wish to have children later. For postmenopausal women, the risk of recurrence being high, endarterectomy is recommended.
Endometrial cancer is a cancer of the inside of the uterus, where the endometrium is the lining that lines the inside of the uterus. In women with cancer at this level, endometrial cells multiply abnormally. Endometrial cancer usually occurs after menopause, but 10 to 15% of cases affect premenopausal women, including 2 to 5% of women under 40 years old.
A significant proportion of endometrial cancer is thought to be attributable to an excess of estrogenic hormones produced by the ovaries or supplied by the outside. The ovaries produce 2 types of hormones during the female cycle: estrogen and progesterone. These hormones act on the endometrium throughout the cycle, stimulating its growth and then its expulsion during menstruation. An excess of estrogen hormones would create an imbalance conducive to the poorly controlled growth of endometrial cells.
Several factors can increase estrogen levels, such as obesity or hormone therapy with estrogen alone. This type of hormone therapy is therefore reserved for women who have had the uterus removed or hysterectomy who are no longer at risk of endometrial cancer. For more information, see the People at risk and Risk factors sections.
For some women, however, endometrial cancer does not appear to be caused by a higher level of estrogen.
Other causes are involved in endometrial cancer, such as advanced age, overweight or obesity, genetics, hypertension, etc.
Sometimes cancer occurs without a risk factor being identified.
Like any mucous membrane, the endometrium is made up of surface cells called “epithelial” and supporting tissue, the “chorion”. More than 90% of endometrial tumors develop at the expense of the epithelium. This category includes cancerous lesions such as adenocarcinomas and carcinosarcomas, pre-cancerous lesions such as atypical hyperplasias, endometrial polyps, and lesions induced by tamoxifen. Adenocarcinomas, the most common form, are developed from "glandular" type epithelial cells.
Other metabolic factors: diabetes and glycemic load
Diabetes is a risk factor for endometrial cancer. The risk of developing this cancer is twice as high (significant relative risk) in diabetic patients than in people without diabetes (Larsson, 2006).
It is the development of insulin resistance that is responsible for the increased risk of cancer. Insulin is then in large quantities in the blood and will be able to stimulate growth factors acting on the endometrium. The precise mechanisms are not well known. This is confirmed in the 2013 WCRF / AIRC report. This same international report also found that increased glycemic load (which estimates the ability of foods eaten to increase blood glucose) is a risk factor for endometrial cancer with a probable level of scientific evidence to account. based on current scientific data; these are not as convincing as for obesity.
Early puberty and late menopause
Age at puberty determines when the ovaries start producing estrogen, and menopause determines when they stop producing estrogen. Earlier puberty or late menopause, therefore, exposes a woman to estrogen for a longer period of her life and therefore represents a risk factor.
Not having had a child (nulliparity)
The menstrual cycle of women experiences a period during which the functional area of the endometrium collapses. In order to accommodate the future fertilized egg, the endometrium must regenerate. For this, estrogen plays a role in stimulating cell growth in the endometrium.
During pregnancy, there is no ovulation for 9 months. The estrogen stimulation does not stop, however, but is much less than if there had been 9 ovarian cycles. Thus, women without children are exposed to greater amounts of estrogen: this is considered a risk factor for the development of endometrial cancer (Lochen, 1997).
This is sort of how polyp can be the root cause of cancer or various tumors.
To contact our experts please call or write to us on the following number, tel / WhatsApp: https://wa.me/22996374527
HYSTEROSCOPY UTERINE POLYPES CURETTING: Natural treatment
UTERINE HYSTEROSCOPY POLYPES CURETTING
Uterine curettage is an operation that involves removing the internal tissue of the uterus called the endometrium.
This curettage is carried out using a curette (a small "spoon"). Here is the natural treatment to cure uterine polyps without curettage. Click on the image below to discover this natural treatment.
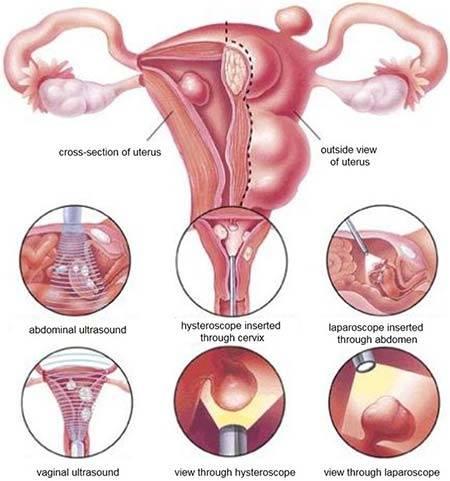
Curettage is most often performed in conjunction with hysteroscopy.
Previously the polyps were removed by an intervention called: Curettage, today this intervention has become obsolete and out of fashion because blind and often incomplete.
Hysteroscopic resection of polyps: consists under visual control (thanks to the endoscope placed in the cavity) in electively (precisely) removing the polyp without touching the rest of the cavity, so as not to damage it (this intervention must replace the classic “curettage” which is now somewhat obsolete because it is blind and often incomplete). This new way of approaching the procedure (the use of an endoscopic camera) is more precise and does not risk impairing subsequent fertility. If the polyps are multiple or numerous, this method makes it possible to list them and remove them all with precision (each will be analyzed separately).
After menopause, or when the patient no longer wishes to become pregnant, it can be combined with an endarterectomy (intervention which consists in removing the endometrium: the mucous membrane that lines the uterus) in order to prevent new polyps from growing nearby. of those who have been withdrawn; this intervention (endarterectomy) clearly improves the results of this type of intervention.
In patients of childbearing age, the operative hysteroscopy should be checked by a new diagnostic hysteroscopic check (done in consultation) one to two months after the operation in order to check the integrity of the cavity and the good healing.
Treatment may not be necessary if the polyps are not causing any symptoms. However, polyps should be treated if they cause heavy bleeding during menstruation or if they are suspected of being precancerous or cancerous. They should be removed if they cause problems during pregnancy, such as miscarriage, or result in infertility in women who wish to become pregnant. If a polyp is discovered after menopause, it should be removed.
The treatment methods include the following:
- Medicines: Medicines that help regulate hormonal balance, such as progestins or gonadotropin-releasing hormone agonists, can be used temporarily. These drugs help relieve symptoms. However, symptoms will usually return after you stop taking the medication.
- Hysteroscopy: (see above) This can also be used as a method of treatment. In treatment, the doctor inserts surgical instruments into the hysteroscope to remove the detected polyps.
- Curettage: (see above) It can be performed at the same time as a hysteroscopy. While using the hysteroscope to examine the inside of the uterus, the doctor uses a curette to scrape the lining and remove polyps. Polyps can be sent to a lab to determine if they are benign or cancerous. This technique is effective for small polyps.
- Additional surgery may be needed if a polyp cannot be removed by other methods or if the polyps are cancerous. A hysterectomy, a surgical procedure that removes the entire uterus, may be needed in cases where cancer cells are found in uterine polyps.
Operative hysteroscopy is the treatment of excellence for the uterine polyp.
The surgical procedure will remove the polyp in its entirety including the area on which the uterine polyp is implanted. Sometimes the adjacent mucosa will also be removed during the same operation, when it is too thick, especially when the patient is postmenopausal. An endometrial resection or endarterectomy will then be performed. When performing a therapeutic curettage, the doctor removes the contents of your uterus, not just a small sample of tissue. Your doctor can do this for:
- Cleanse the tissues that remain in the uterus after a miscarriage or abortion to prevent infection or heavy bleeding
- Remove a molar pregnancy, in which a tumor forms instead of a normal pregnancy
- Treat excessive bleeding after childbirth by clearing the placenta from the uterus
- Remove cervical or uterine polyps, which are usually non-cancerous (benign)
Curettage with another procedure called a hysteroscopy. During a hysteroscopy, thin with a light and a camera at the end into your vagina, through your cervix, and into your uterus.
The doctor then views the lining of your uterus on a screen, noting any areas that appear abnormal, checking for polyps, and taking tissue samples, if necessary. During a hysteroscopy, your doctor may also remove uterine polyps and fibroids.
This polyp will be sent to the laboratory which will analyze it; in a few days, the result will be available. But the surgeon is most often able to guide the diagnosis and reassure the patient at the simple macroscopic view during the operation (i.e. with the simple eye) of the nature of this polyp
For dilation and curettage, you will be given anesthesia. The choice of anesthesia depends on the reason for curettage and your medical history.
General anesthesia makes you unconscious and unable to feel pain. Other forms of anesthesia provide light sedation or injections to numb only a small area (local anesthesia) or a larger area (regional anesthesia) of your body.
During the procedure:
- Your doctor inserts an instrument called a speculum into your vagina, like during a Pap test, to see your cervix.
- Your doctor inserts a series of thicker and thicker sticks into your cervix to slowly dilate your cervix until it is properly opened.
- Your doctor removes the dilation rods and inserts a spoon-shaped instrument with a sharp edge or suction device, then removes the uterine tissue.
Because you are unconscious or sedated during D&C, you should not experience any discomfort.
After the procedure
You can spend a few hours in a recovery room after the D&C so your doctor can monitor you for heavy bleeding or other complications. It also gives you time to recover from the effects of the anesthesia.
If you had general anesthesia, you might feel nauseous or vomit, or you might have a sore throat if a tube was placed in your windpipe to help you breathe. With general anesthesia or light sedation, you may feel drowsy for several hours.
The normal side effects of a D&C can last for a few days and include:
- Slight cramps
- Spotting or light
- Postoperative check-up: very rarely, a new diagnostic hysteroscopy will be performed after surgery to assess the state of the uterine cavity. Most often no examination is necessary following the removal of a polyp by operative hysteroscopy.
Of course, if the results of the polyp analysis are worrying, a new medical and surgical strategy will be considered.