UTERINE HYSTEROSCOPY POLYPES CURETTING
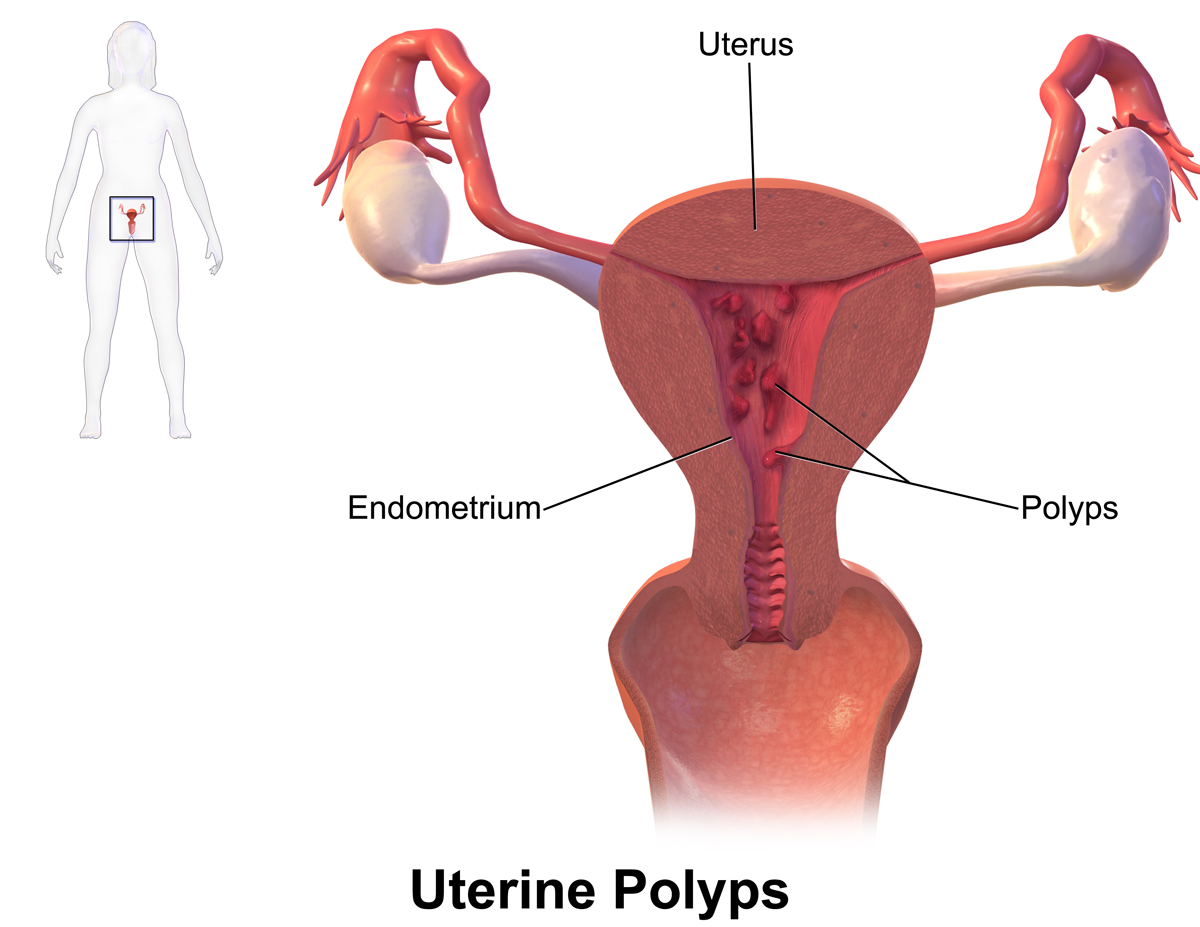
Uterine curettage is an operation that involves removing the internal tissue of the uterus called the endometrium.
This curettage is carried out using a curette (a small "spoon"). Here is the natural treatment to cure uterine polyps without curettage. Click on the image below to discover this natural treatment.
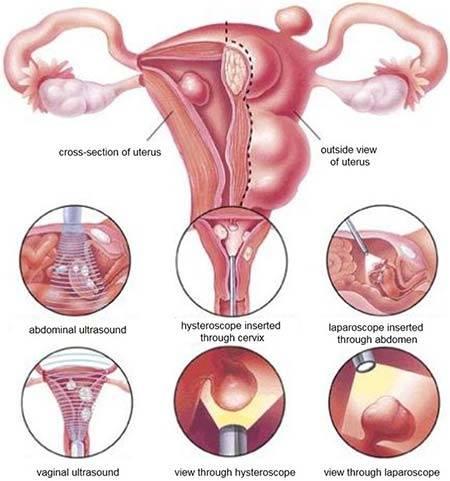
Curettage is most often performed in conjunction with hysteroscopy.
Previously the polyps were removed by an intervention called: Curettage, today this intervention has become obsolete and out of fashion because blind and often incomplete.
Hysteroscopic resection of polyps: consists under visual control (thanks to the endoscope placed in the cavity) in electively (precisely) removing the polyp without touching the rest of the cavity, so as not to damage it (this intervention must replace the classic “curettage” which is now somewhat obsolete because it is blind and often incomplete). This new way of approaching the procedure (the use of an endoscopic camera) is more precise and does not risk impairing subsequent fertility. If the polyps are multiple or numerous, this method makes it possible to list them and remove them all with precision (each will be analyzed separately).
After menopause, or when the patient no longer wishes to become pregnant, it can be combined with an endarterectomy (intervention which consists in removing the endometrium: the mucous membrane that lines the uterus) in order to prevent new polyps from growing nearby. of those who have been withdrawn; this intervention (endarterectomy) clearly improves the results of this type of intervention.
In patients of childbearing age, the operative hysteroscopy should be checked by a new diagnostic hysteroscopic check (done in consultation) one to two months after the operation in order to check the integrity of the cavity and the good healing.
Treatment may not be necessary if the polyps are not causing any symptoms. However, polyps should be treated if they cause heavy bleeding during menstruation or if they are suspected of being precancerous or cancerous. They should be removed if they cause problems during pregnancy, such as miscarriage, or result in infertility in women who wish to become pregnant. If a polyp is discovered after menopause, it should be removed.
The treatment methods include the following:
- Medicines: Medicines that help regulate hormonal balance, such as progestins or gonadotropin-releasing hormone agonists, can be used temporarily. These drugs help relieve symptoms. However, symptoms will usually return after you stop taking the medication.
- Hysteroscopy: (see above) This can also be used as a method of treatment. In treatment, the doctor inserts surgical instruments into the hysteroscope to remove the detected polyps.
- Curettage: (see above) It can be performed at the same time as a hysteroscopy. While using the hysteroscope to examine the inside of the uterus, the doctor uses a curette to scrape the lining and remove polyps. Polyps can be sent to a lab to determine if they are benign or cancerous. This technique is effective for small polyps.
- Additional surgery may be needed if a polyp cannot be removed by other methods or if the polyps are cancerous. A hysterectomy, a surgical procedure that removes the entire uterus, may be needed in cases where cancer cells are found in uterine polyps.
Operative hysteroscopy is the treatment of excellence for the uterine polyp.
The surgical procedure will remove the polyp in its entirety including the area on which the uterine polyp is implanted. Sometimes the adjacent mucosa will also be removed during the same operation, when it is too thick, especially when the patient is postmenopausal. An endometrial resection or endarterectomy will then be performed. When performing a therapeutic curettage, the doctor removes the contents of your uterus, not just a small sample of tissue. Your doctor can do this for:
- Cleanse the tissues that remain in the uterus after a miscarriage or abortion to prevent infection or heavy bleeding
- Remove a molar pregnancy, in which a tumor forms instead of a normal pregnancy
- Treat excessive bleeding after childbirth by clearing the placenta from the uterus
- Remove cervical or uterine polyps, which are usually non-cancerous (benign)
Curettage with another procedure called a hysteroscopy. During a hysteroscopy, thin with a light and a camera at the end into your vagina, through your cervix, and into your uterus.
The doctor then views the lining of your uterus on a screen, noting any areas that appear abnormal, checking for polyps, and taking tissue samples, if necessary. During a hysteroscopy, your doctor may also remove uterine polyps and fibroids.
This polyp will be sent to the laboratory which will analyze it; in a few days, the result will be available. But the surgeon is most often able to guide the diagnosis and reassure the patient at the simple macroscopic view during the operation (i.e. with the simple eye) of the nature of this polyp
For dilation and curettage, you will be given anesthesia. The choice of anesthesia depends on the reason for curettage and your medical history.
General anesthesia makes you unconscious and unable to feel pain. Other forms of anesthesia provide light sedation or injections to numb only a small area (local anesthesia) or a larger area (regional anesthesia) of your body.
During the procedure:
- Your doctor inserts an instrument called a speculum into your vagina, like during a Pap test, to see your cervix.
- Your doctor inserts a series of thicker and thicker sticks into your cervix to slowly dilate your cervix until it is properly opened.
- Your doctor removes the dilation rods and inserts a spoon-shaped instrument with a sharp edge or suction device, then removes the uterine tissue.
Because you are unconscious or sedated during D&C, you should not experience any discomfort.
After the procedure
You can spend a few hours in a recovery room after the D&C so your doctor can monitor you for heavy bleeding or other complications. It also gives you time to recover from the effects of the anesthesia.
If you had general anesthesia, you might feel nauseous or vomit, or you might have a sore throat if a tube was placed in your windpipe to help you breathe. With general anesthesia or light sedation, you may feel drowsy for several hours.
The normal side effects of a D&C can last for a few days and include:
- Slight cramps
- Spotting or light
- Postoperative check-up: very rarely, a new diagnostic hysteroscopy will be performed after surgery to assess the state of the uterine cavity. Most often no examination is necessary following the removal of a polyp by operative hysteroscopy.
Of course, if the results of the polyp analysis are worrying, a new medical and surgical strategy will be considered.